|
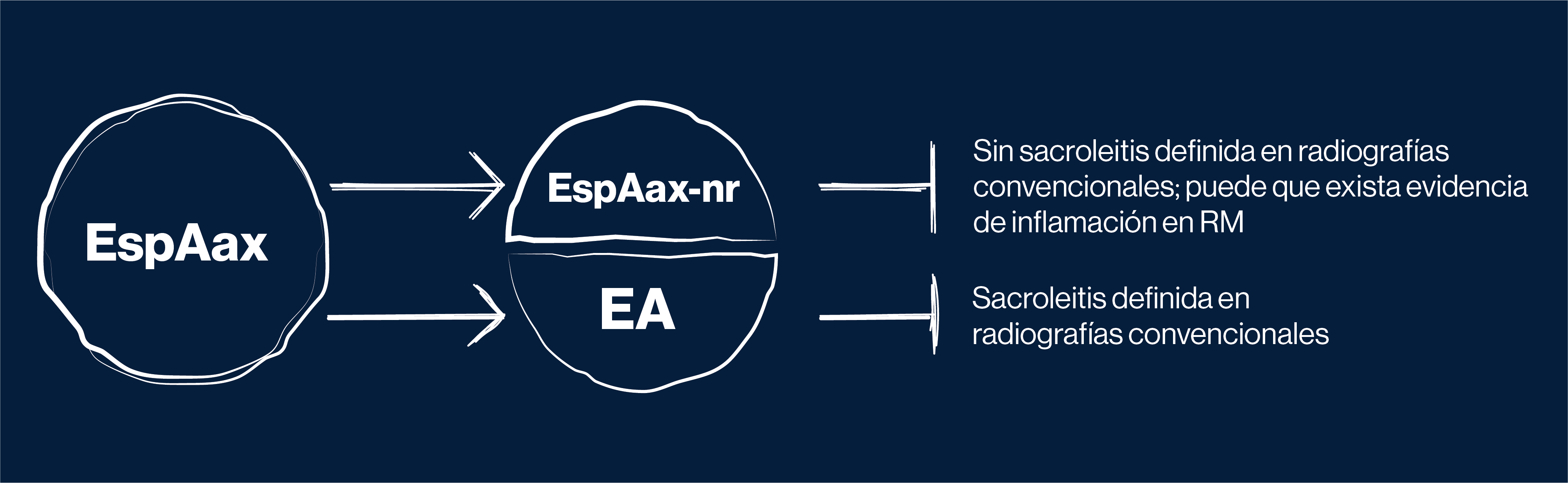
Con el tiempo, es probable que al menos un 50% de los pacientes con EspAax-nr progresen a EA.2
|
Entre los factores de riesgo para la progresión se incluyen:2
|
HLA-B27 positivo |
Actividad inflamatoria elevada: - PCR elevada- RM que muestre inflamación de las articulaciones sacroilíacas |
Dolor de nalgas
|
|
Hábito fumador |
Historia de uveítis |
Sacroileítis de bajo grado
|
|
La EspAax puede convertirse en una pesadilla para los pacientes, independientemente de que puedas verla en las radiografías convencionales o no.
|
EA: espondilitis anquilosante; EspAax: espondiloartritis axial; EspAax-nr: espondiloartritis axial no radiográfica; HLA: antígeno leucocitario humano (por sus siglas en inglés); PCR: proteína C reactiva; RM: resonancia magnética.
|
|
|
Referencias:
1. Rudwaleit M, et al. The development of Assessment of SpondyloArthritis International Society classification criteria for axial spondyloarthritis (part II): validation and final selection. Ann Rheum Dis. 2009;68:777–783; 2. Protopopov M, Poddubnyy D. Radiographic progression in non-radiographic axial spondyloarthritis. Expert Rev Clin Immunol. 2018;14:525–533; 3. Mease PJ, et al. Characterization of patients with ankylosing spondylitis and nonradiographic axial spondyloarthritis in the US-based Corrona Registry. Arthritis Care Res (Hoboken). 2018;70:1661–1670; 4. Strand V, Singh JA. Evaluation and management of the patient with suspected inflammatory spine disease. Mayo Clin Proc. 2017;92:555–564; 5. Kiltz U, et al. Do patients with non-radiographic axial spondylarthritis differ from patients with ankylosing spondylitis? Arthritis Care Res (Hoboken). 2012;64:1415–1422; 6. Malaviya AN, et al. Comparison of patients with ankylosing spondylitis (AS) and non-radiographic axial spondyloarthritis (nr-axSpA) from a single rheumatology clinic in New Delhi. Int J Rheum Dis. 2015;18:736–741; 7. Boonen A, et al. The burden of non-radiographic axial spondyloarthritis. Semin Arth Rheum. 2015;44:556–562; 8. Rudwaleit M, et al. The challenge of diagnosis and classification in early ankylosing spondylitis: do we need new criteria? Arthritis Rheum. 2005;52:1000–1008; 9. Sieper J, et al. Axial spondyloarthritis. Nat Rev Dis Primers. 2015;1:15013; 10. Vidal C, et al. Poor efficacy of TNF inhibitors in non-radiographic axial spondyloarthritis in the absence of objective signs: a bicentric retrospective study. Joint Bone Spine. 2018;85:461–468; 11. Chakrabarty S, Zoorob R. Fibromyalgia. Am Fam Physician. 2007;76:247–254; 12. Sieper J, Rudwaleit M. Early referral recommendations for ankylosing spondylitis (including pre-radiographic and radiographic forms) in primary care. Ann Rheum Dis. 2005;64:659–663; 13. Rusman T, et al. Gender differences in axial spondyloarthritis: women are not so lucky. Curr Rheumatol Rep. 2018;20:35; 14. Baraliakos X, et al. Patients with fibromyalgia rarely fulfil classification criteria for axial spondyloarthritis. Rheumatology (Oxford). 2018;57:1541–1547; 15. Lee W, et al. Are there gender differences in severity of ankylosing spondylitis? Results from the PSOAS cohort. Ann Rheum Dis. 2007;66:633–638.

